|
TRANSLATE THIS ARTICLE
Integral World: Exploring Theories of Everything
An independent forum for a critical discussion of the integral philosophy of Ken Wilber
 Andrew P. Smith, who has a background in molecular biology, neuroscience and pharmacology, is author of e-books Worlds within Worlds and the novel Noosphere II, which are both available online. He has recently self-published "The Dimensions of Experience: A Natural History of Consciousness" (Xlibris, 2008). Andrew P. Smith, who has a background in molecular biology, neuroscience and pharmacology, is author of e-books Worlds within Worlds and the novel Noosphere II, which are both available online. He has recently self-published "The Dimensions of Experience: A Natural History of Consciousness" (Xlibris, 2008). SEE MORE ESSAYS WRITTEN BY ANDY SMITH When Those Who Save Become Those Who KillDe-Bunking Andrew Cuomo's Nursing Home ScandalAndy Smith
NY has been touted by the liberal press as an example of a state that, after a horrific start, is doing the right things to bring the virus under control.
The first documented case of COVID-19 appeared in the U.S. in the third week of January, 2020. Cases began to accumulate in February, and by early March, New York City became an epicenter, daily recording more new cases and more deaths than in any other city in the U.S. Indeed, it soon outstripped Wuhan, the Chinese city where the pandemic began. Since New York City is the hub of a megapolis on the northeast coast of the U.S., which stretches into the neighboring states of Massachusetts (MA), Connecticut (CT), Rhode Island (RI) and New Jersey (NJ), these states, along with New York state, all became a hotbed for spread of the virus. 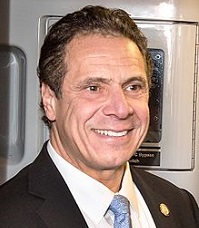 Andrew Cuomo The governors of these states, and particularly Andrew Cuomo of New York, felt the pressure of an impending collapse of the hospital system to care for these patients. That collapse, thankfully, for the most part did not happen, but while the cases and deaths were growing, Cuomo, and several other governors, took a risky step intended to alleviate the impending shortage of beds for hospital patients. They ordered nursing homes (NH), or long-term care facilities, to accept the transfer of some of these hospital patients. This was potentially dangerous, because these NH house their residents in a relatively small space, increasing the probability of virus transmission, and because these residents are old and generally suffer from various medical conditions, which puts them at significantly high risk for dying from the virus. Introducing recovering COVID-19 patients into them appeared to be like throwing a match into a tank of gasoline. Sure enough, nursing home deaths began to rise in these states at the time. These were not the only states to experience this problem. The first recorded death from COVID-19 occurred in a NH in Washington state, on the opposite, west coast of the U.S. In fact, as an analysis reported in Forbes in late May showed, every state in the U.S has had NH deaths. It's now recognized as a problem all over the country. According to the Forbes analysis, nearly half of all deaths from COVID-19 have occurred in NH. But the highest amount of NH deaths occurred in NY, followed by NJ. Other states with very high death totals, such as MA, CT, and RI, also had been transferring hospital patients. This led many observers to conclude that many if not most of these deaths were the result of these hospital patients introducing the virus into what had previously been a safe environment. This became a politically-charged subject, because most of the states that ordered these transfers have Democratic governors, though MA (despite being a “blue state”, which votes reliably Democratic in Presidential elections) is an exception. Eventually, the public outcry became so great that all such transfers were stopped. But the blame game has not. Even now, virtually every day there is a new article by a conservative commentator in which Cuomo's guilt is held up to him. This has gone on even as NY, NJ and other northeastern states are actually reporting fewer cases and fewer deaths than other areas of the U.S., particularly the south and west, where new cases are now spiking. NY has been touted by the liberal press as an example of a state that, after a horrific start, is doing the right things to bring the virus under control. The current numbers support this, while the right wing continues to blame Cuomo. The blame, though, is misplaced. The notion that nursing home deaths resulted from transfer of hospital patients is a myth, propagated by journalists who don't follow the science very closely. Let's see why. How long are COVID-19 patients infectious?It has been about six months since Chinese officials, and eventually, the rest of the world, recognized that a new virus, SARS-CoV-2, was responsible for a highly contagious illness that was a major threat to the public. During that time, we have learned a lot of important things about the virus. We know its RNA sequence, as Frank has pointed out. We understand, fairly well, how the virus is transmitted from person to person—mostly through airborne particles emitted by breathing or coughing by infected individuals. We know the molecular steps involved in the viral entry into host cells. We know many of the symptoms of infection, though we don't fully understand the processes involved in some of the most serious ones. We know how long it takes after infection for these symptoms to appear. This information is vital to our approach to controlling the pandemic. Knowing the RNA sequence enables us to devise a PCR test that determines whether someone has the virus. Knowing that the virus is transmitted through the air is the basis of social distancing and wearing face masks. Knowing how the virus enters cells is critical to developing antibodies that can prevent the virus from doing this. Knowing that symptoms usually emerge within a few days after infection, but in some cases, not until two weeks later, is the basis for quarantining people of unknown status for fourteen days. One very basic and important issue we don't have a lot of information about, though, is how long an infected person remains infectious—that is, capable of infecting another person. We would like to know more about this period, because of course we want to know when an infected person can safely be around others who aren't infected. Currently, recovery from COVID-19 is defined by most reporting agencies as having occurred when the individual no longer exhibits symptoms, and tests negative for the virus twice[1]. If the person no longer has detectable virus in the body, he or she will no longer be a risk of spreading it to someone else, of course. But the converse is not true. A positive PCR test does not mean that someone is necessarily infectious. Why not? The test only determines viral sequence, not active, infectious virus. After the body's immune system begins fighting off the infection, many of the viral particles will become degraded. They may still possess enough sequence to test positive by PCR, even though they no longer are capable of infecting cells—in that individual nor anyone else. The viral sequences are like dead soldiers lying on a battlefield. We can count and identify the bodies, but they are no longer a threat to the opposing army. This important distinction, in fact, created a stir several months ago, when several hundred South Koreans who had tested positive for the virus, and subsequently recovered, tested positive a second time. This seemed to indicate it was possible to become infected more than once. On further analysis, though, the scientists concluded that the PCR test simply revealed the presence of the original virus, now degraded. Such degraded virus can probably persist for some time in most individuals. One early study by researchers in Wuhan reported the presence of viral RNA in individuals for an average of about three weeks after symptoms emerged, and in one individual, as long as five weeks (Zhou et al 2020). This could indicate that these individuals were infectious during that time, but clearly this kind of study doesn't settle the issue. Another study did take the step of attempting to measure active virus, and reported that none was detectable more than eight days after symptoms began (Wolfel et al 2020). However, this method requires that the virus be shown to infect cultured cells, and relatively small amounts of active virus might be difficult to detect in this manner. Certainly any test involving cultured cells is nowhere nearly as reliable nor as sensitive as that detecting sequence, like PCR. So the researchers used a clever trick to answer this question in another way that does involve sequence detection. They measured levels of what is called subgenomic mRNA. When the virus replicates in the host cell, it first produces messenger RNA (mRNA), which is a copy of the genomic RNA—the entire program for making a new virus—in the original virus. This mRNA is then converted, or translated, into the proteins that compose the shell of the virus. The proteins and the newly created copies of genomic RNA are finally assembled into a new virus, identical to the original. The sequences of mRNA are only temporary, though, and differ in certain ways from the genomic RNA of the virus. By assaying these, therefore, the researchers could determine whether the virus was actually active at the time. An active virus, capable of infecting other people, will produce this subgenomic mRNA. A degraded virus will not. These researchers analyzed subgenomic RNA in both the upper respiratory tract, by taking samples from the throat, and the lower respiratory tract, in sputum samples. They reported that active virus was present in the throat for up to just five days after symptoms emerged, while it was present in sputum up to ten days. These results, roughly consistent with the eight day window found when culturing live virus, suggests that infected individuals don't remain infectious for very long after symptoms appear. Infection of other people would mostly occur from virus present in the upper respiratory tract, released into the air through breathing and coughing. One would not expect active virus in the lower tract to be a serious risk to others, unless the individual were constantly spitting at them! The authors concluded, very conservatively: In a situation characterized by a limited capacity of hospital beds in infectious disease wards, there is pressure for early discharge after treatment. On the basis of the present findings, early discharge with ensuing home isolation could be chosen for patients who are beyond day�10 of symptoms and have less than 100,000�viral RNA copies per ml of sputum. Both criteria predict that there is little residual risk of infectivity, on the basis of cell culture. A very different approach, one not requiring any actual analysis of virus, was used by another research group in China (He et al 2020). These scientists began by estimating the length of two intervals: 1) the incubation period, that is, the average time between infection and appearance of the first symptoms; and 2) the serial interval, defined as the average time between infection of one individual and infection by that individual of other individuals. The latter was obtained through analysis of contract tracing, where one infected individual could be definitively shown to have infected another individual at a certain time and place. Both of these estimates take the form of a graph, in which the percentage of some phenomenon—first symptoms, or infection of another individual—is plotted vs time, in days. When one combines the data in these two graphs—infection to symptoms and infection to infection—the result is a plot of infectivity vs. time after emergence of symptoms. The resulting graph revealed a rather stunning conclusion. Infectivity actually begins before the appearance of symptoms, and peaks about sixteen hours before the symptoms emerge. It then rapidly declines, so that it's mostly gone by a week after symptoms emerge. This finding supports the conclusion of presymptomatic transmission of the virus, and of course has major implications for contact tracing, since it implies that many people may spread the virus before they can know they have it. While one would not expect presymptomatic transmission of virus to be so high—after all, a lot of the spread is thought to be due to coughing—this is consistent with the high contagiousness of the virus. It will spread faster if people who are spreading it aren't aware that they're infected. In fact, this is a possible criticism of this approach. Infectivity may be higher before symptoms emerge, and decline soon after, not entirely for physiological reasons—there is less of the virus to spread—but in part for social ones: a person with symptoms may reduce interactions with others. However, the general form of the curve is consistent with the other study I discussed. Together, both these studies, using three different approaches, come to the conclusion that infectiousness mostly runs its course within a week to ten days after symptoms first appear. To conclude, the available studies we have strongly suggest that infectiousness of COVID-19 patients doesn't last very long. This conclusion needs to be confirmed by larger studies in which active virus is measured directly, but we can say for now that there is no evidence that patients ready to be discharged from a hospital would be of risk to other patients in a nursing home. People typically don't even go to a hospital until their symptoms have persisted for several days or more, and they would not be eligible for discharge unless the worst of these symptoms had run their course. To this point, we can add that no study I'm aware of has demonstrated, through contact tracing, that a hospital patient transferred to a nursing home ever infected anyone else in that institution. This despite the fact that much testing—not thorough, in many cases, but still producing a lot of data—of everyone entering a NH has been conducted. Absence of evidence is not evidence of absence, of course, and these findings certainly shouldn't be taken as justifying transfer of recovering COVID-19 patients to nursing homes. But the burden of proof surely should fall on those who claim, after the fact, that hospital patient transfers caused nursing home deaths. COVID-19 and population densityIf NH deaths are not the result of transfer of hospital patients, what has caused them? I pointed out earlier that NY, which aggressively proceeded with such transfers, has the most NH deaths in the U.S. Right up there with NY are states like NJ, MA, CT and RI, which also ordered NH to accept such transfers. These five states have the highest number of NH deaths as a percentage of total population of NH residents.[2] What undercuts this implied connection, though, is the fact that NY also has the most COVID-19 deaths outside of nursing homes. In fact, as of late May, when the Forbes analysis I referred to earlier was published, there were forty-four states that reported NH deaths, and when I compared state-by-state the number of deaths inside and outside of NH[3], the correlation was 0.87. In other words, whatever factors are driving deaths within NH must also be driving them outside. That obviously can't be transfer of hospital patients, since many, in fact most states, did not allow such transfers, so what's going on? The fact that so many of these deaths have occurred in the northeast corridor of the U.S. should point to an obvious factor: population density (PD). NYC has by far the highest PD of any city in the U.S., and the top four states are NJ, RI, MA and CT—the same four, along with NY state, that reported the highest rates of NH deaths. Logically, one would expect that a disease transmitted through social interactions would thrive in the densest populations, and in fact, I confirmed that there is a strong correlation of PD (0.75 � 0.80) with both case rate (cases per million) and death rate (deaths per million) throughout the U.S.[4] Now we can focus on the real villain (or unsuspecting patsy) in this crime. It's the staff who work in NH. They come and go every day, which means they are constantly exposed to the risk of contracting the virus in the surrounding community. The higher the case rate in this surrounding community, the greater the likelihood that these staff will become infected, and thus potentially infect the patients they are charged with taking care of. In the early phase of the pandemic, visitors to NH would also be a risk, but they were soon banned. Staff, of course, have to work there. Do we have any evidence for this other than the correlation of NH deaths with case rates in the surrounding community? We certainly know that the staff working in many NH have contracted the virus, and some have died from it. In fact, when states report NH deaths, they generally distinguish between those of residents, and those of staff. The number of staff deaths is far lower, which is to be expected, not only because residents greatly outnumber staff, but because staff members are generally younger and in better health, and thus at less risk for dying from the virus than the residents are. Staff infections don't prove that they were the source of resident infections. But we can also consider states with high overall case and death rates that did not transfer hospital patients, and conversely, states with low overall rates that did transfer them. MA is an example of the former. Though the state did initially order transfer of hospital patients to NH, it soon reversed course, as a result of public pressure. Despite this, it has one of the highest rates of NH deaths—that is, deaths as a % of the total NH population—in the country. By late May, more than 10% of the residents of MA NH had died. Part of this may be attributable to problems in testing staff and residents but the high rate also is consistent with the high case rate in the state. California (CA) is an example of the second situation. Like NY and NJ, the state ordered NH to accept hospital transfers, though it subsequently allowed some exceptions. In any case, at the end of May, the state one of the lowest rates of NH deaths in the U.S.—less than 1.5%. Though CA is by far the most populous state in the union, that population is relatively spread out, particularly in Los Angeles and in the rest of the southern part of the state. San Francisco has a very high population density—in fact, it's second only to NYC—but it contributes much less population to the entire state. Also, it's salient to note that SF's mayor, London Breed, was one of the first big city mayors in the country to impose restrictive measures early in the pandemic, which has played a major role in keeping the case rate there relatively low. Other states that ordered NH to accept hospital patients include Pennsylvania (PA), Illinois (IL), Michigan (MI), and Minnesota (MN)—yes, all of them have Democratic governors! These four states have moderately high NH death rates (3-5%, at the end of May)5. PA incudes part of the NE corridor, with Philadelphia the fifth most population dense city (> 500,000 people) in the U.S., and Chicago in Illinois is another highly dense city (fourth highest). So their NH death rates would be expected to be somewhat elevated relative to that of other parts of the country. But their state-wide NH death rates were less than half of those of NJ, CT and MA, states have higher population densities more than twice as high. In concluding this, I want to emphasize that analysis of NH death rates is complicated by the fact that they are of course strongly affected by how thoroughly these institutions test staff and residents. At some point during the pandemic, state governments realized that they had to test both staff and residents regularly to protect them, and there has been a lot of variability in procedures from state to state. I previously mentioned MA in this regard, and RI is another state with a very high NH death rate that has been plagued with testing shortfalls. Also, some states may have modified their orders in various ways, in an attempt to protect NH residents. I mentioned CA in this connection earlier. That said, the parallel of deaths within NH with case rates and population densities surrounding them is striking, and the latter must be considered a major factor in these deaths.[6] The very strong link of PD with case and death rates has another important political implication. Most of the states with the highest PD, as I noted earlier, are in the NE corridor, and virtually all of them are blue, or Democratic states. The exceptions are MA and Maryland (MD), and that is only because they currently have a Republican governor. Both states are essentially certain to vote Democratic in the coming election. Most red states are concentrated in the south, with many also in the Midwest and west, and they generally have much lower PD. Even highly populated red states in the south, such as Florida (FL) and Texas (TX) have populations that are relatively diffuse. TX boasts five of the fifteen most populated cities in the U.S., yet they have a combined population less than that of NYC. Florida (which could be considered purple, or about even politically, but which does have a Republican governor currently) ranks eighth among states in PD, but it has only one city with a population of greater than 500,000, and that has a very low PD relative to other large cities. Cities and their surrounding metropolitan areas are the primary drivers of the pandemic. This blue vs. red difference isn't a coincidence. States with lower PD tend to be more conservative, because in rural and other relatively sparsely populated areas, the kinds of issues that have driven liberal programs—large immigrant and other ethnic populations, poverty, crime—have been less pressing, at least until recently. Older values are associated with older ways of life, and these ways of life are more common far away from large urban areas. But a result of this is that red states tend to have much lower case rates than blue states. This makes it appear that these states have handled the pandemic, on the whole, better, when a closer examination suggests that they've mostly been lucky, in that their populations are not as favorable to spread of the virus as more densely packed regions of the country. The spike in cases most of these states are now experiencing is probably in large part because the people running them didn't appreciate this, and thought they had succeeded in controlling the virus to a far greater extent than has actually been the case. A new nursing home crisis?If NH deaths are largely tied to the spread of the virus in the communities surrounding these institutions, then their residents are still at risk as the spread of the virus continues. As I noted earlier, NY and other states in the NE corridor have greatly reduced the number of new daily cases, but this is not the case for much of the rest of the country, particularly the south and the west. Cases have spiked in North Carolina, Georgia, Florida, Louisiana, Texas, Arizona, and California, among other states. Writing recently in The Atlantic, Olga Khazan warns that a new nursing home crisis may result if this trend continues. Echoing the point I've made here, she notes: Some experts say�the best way to stop coronavirus outbreaks inside nursing homes, then, is to stop them�outside�of nursing homes first. But state and federal leaders have largely failed to do that too. We can see the results of this in some of the states now undergoing surges in the virus. Florida, whose Governor, Ron DiSantis, was hailed by the conservative press for resisting the temptation to transfer hospital patients to NH, nevertheless featured a typical 43% of its total deaths in NH at the end of May. Since then, the state has added about 1500 more deaths, about 600 of which have occurred in NH—the same rate as before. Georgia has added about 900 more deaths, a little over one-third of which have been NH residents. AZ has added more than 1000 deaths, though a little less than 20% of those are NH residents. Even the NE states, which have reduced their new cases and deaths dramatically recently, have seen significant increases over this entire period. NJ has reported about 2300 new deaths—though declining steadily since the beginning of June—about 30% of which were in NH. These data suggest that the risk for residents in NH is still substantial.[7] The overall death rate in the U.S., however, has been declining for more than two months, a fact used by those favoring more loosening of restrictions as evidence that the worst of the pandemic is over. It has been a striking feature that even as the absolute number of daily new cases in the U.S. has increased to record levels, the number of deaths has declined to about 20% of what it was at its peak. Part of the reason for this may be that deaths lag beyond cases by several weeks. We will learn soon enough how much of a factor this is. It's also very likely that most of the new cases are relatively young people, who are at very low risk of dying. Rebekah Jones, formerly Florida's chief data scientist, who was fired, she claims, for refusing to manipulate data that would make the state's situation look better, connects the surge to more young people returning to jobs as the economy opens up. Whatever the reasons, though, increasing numbers of cases are likely to reach the older, more vulnerable population sooner or later. As long as the caregivers staffing nursing homes are at risk when outside of these institutions, it's inevitable that the people whose lives they're charged with to improve will be at risk as well. Endnotes[1] Two tests are important, chiefly because the PCR test for the virus often produces false negatives. This does not reflect a flaw in the test per se, which is very reliable. The problem is that it can be difficult to extract virus from deep in the nasal cavity. [2] To determine the number of deaths in nursing homes, I multiplied total reported COVID-19 deaths in each state by the % of deaths in nursing homes that was reported by Forbes. Total population of NH residents was taken from: www.kff.org [3] NH deaths and total deaths were determined as described in note 2. [4] I performed this analysis initially at the end of May, and repeated it with updated data several weeks later. [5] MI did not report NH deaths at the time of the Forbes analysis. It has done so subsequently, though, and even using the current total, which would be expected to be higher than that at the end of May, the number of NH deaths as a proportion of the total NH population in the state is about 5.2%. It drops to 4.8% for the end of May if we assume NH deaths increased during the period from then to now at the same rate as overall deaths. [6] I don't mean to claim that high PD is always associated with high case and death rates of the virus. Tokyo has one of the highest PD in the world, and has a very low rate of cases and deaths. Even more remarkably, other factors that in most countries are believed to have had major beneficial effects—such as government interventions and testing of the population—are minimal. Speculation on how the Japanese have kept the virus relatively at bay is beyond the scope of this paper, but PD density has a strong correlation with spread of the virus throughout the U.S., because many other possible factors have tended to be more or less the same, at least until some states began loosening restrictions. It's also worth noting that the effects of PD are clearly evident in Europe. Of the half dozen or so European nations that have a higher COVID-19 death rate than the U.S., all but one of them has a much higher PD than the U.S. The exception is Sweden, one of the few countries in the world not to have a lockdown. While all these European countries have succeeded more than the U.S. in bringing the virus under control, they initially experienced very high numbers of cases and deaths, and high PD was unquestionably a major factor. [7] Nursing home deaths are still not reported by all states, and those that do frequently furnish them only in very long tables documenting deaths in every one of hundreds of institutions, making determining totals difficult and frustrating. The examples I've provided here have been drawn from state dashboards that furnished the information more transparently. To add to the problems, death totals are frequently revised over time, so comparisons of totals on one date with those on another may not be perfectly accurate. But the numbers I provide here are only intended to provide a rough idea of what has happened. ReferencesHe, X., et al. (2020) Temporal dynamics in viral shedding and transmissibility of COVID-19. Nature Medicine 26, 672-675 W�lfel, R. et al. (2020) Virological assessment of hospitalized patients with COVID-2019.�Nature 581, 465-469 Zhou, F. et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study.�Lancet�395, 1054�1062
|